By Dr Hassan Mubark
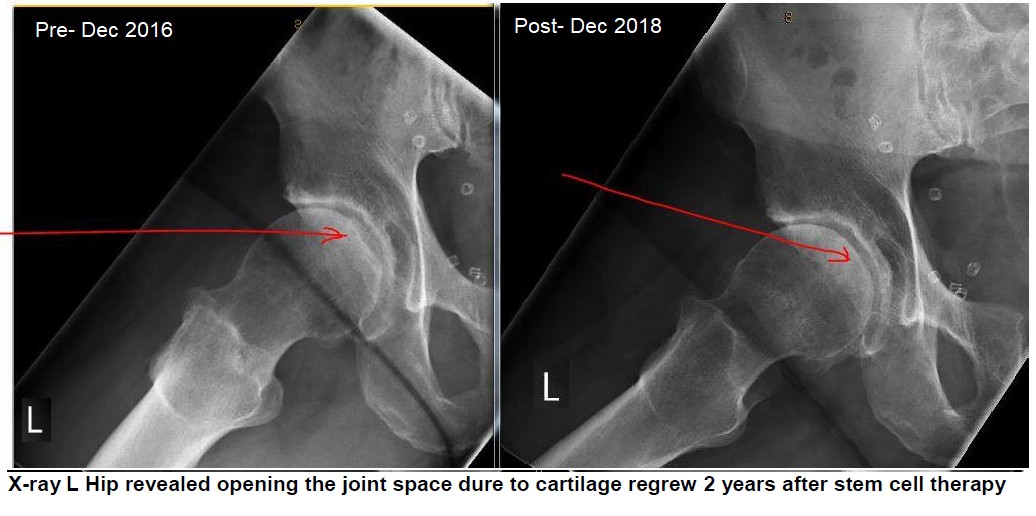
A 69-year-old male who presented with bilateral hip pain associated with stiffness and clicking sensation. He had stem cell therapy in February 2018 for both hips. The left one has more symptoms than the right one, with the x-rays in December 2016 revealing a severely narrowed hip on the left side and the right side, he had early degenerative changes.
As per the initial protocol for stem cell therapy at that time, he had two injections six months apart in the hips; the 1st one was in March 2018 and the 2nd injection in September 2018 for both hips to help his osteoarthritis. He was followed up in November 2018, and he reported no pain in the right hip at all but he had a little bit of pain remaining on the left side. Examination of the left side revealed mild restriction in both internal and external rotation with no significant tenderness, and he was happy with the outcome. Given the severity of the osteoarthritis in the left hip, he requested to have a repeat of the x-ray to show the changes in the hip joint, and this was repeated in December and showed mild changes in the right hip, and the left hip showed moderate cartilage loss. This was compared to 2016, which was severe osteoarthritis. This means there is some cartilage regeneration.
So far, he is pain-free with a good range of motion of the hips, and no pain killers are required. He will do well despite the severity of osteoarthritis in the left hip. He will no longer need surgery, and the reason he decided to have the 2nd injections for the hips was to make sure that he wouldn't need surgery. For severe cases, the protocol requires two injections six months apart. The current protocol, if mild or moderate or early severe, is a one-off injection. In this case, the prognosis for the right hip is 100 % good, but the joint will show more regeneration for the left one, as illustrated in the x-rays. The client was very appreciative of these excellent results.
By Dr Hassan Mubark
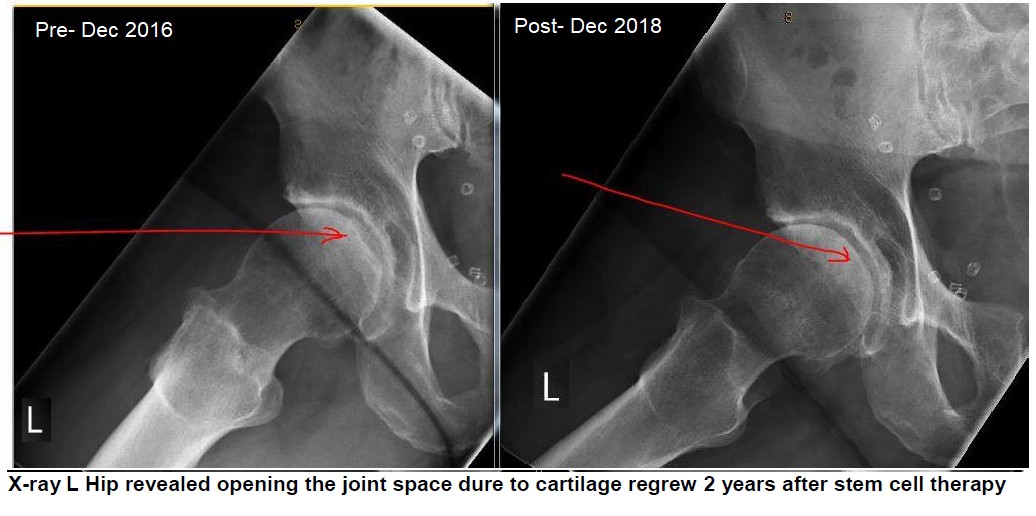
A 54-year-old male involved in active sports and attending the gym regularly. He does karate and martial arts. He had a significant injury to his right knee in September 2018, and he was seen by the orthopedic surgeon with symptoms of significant pain and limitation of movement and knee swelling.
His MRI showed the following:
Before Oct 2018
1. Progressive tearing of the medial meniscus with further maceration of the posterior horn and body and newly displaced flaps
2. Progressive chondral damage of the central and posterior weight-bearing medial femoral condyle, now with areas of full-thickness cartilage loss
3. Large knee joint effusion and moderate Baker's cyst
After stem cells Aug 2019
1. No significant change in appearances of the medial meniscal tear involving posterior horn and posterior body
2. The full-thickness chondral defect at the medial femoral condyle is also similar
3. Decreased joint fluid volume and almost complete resolution of previous Baker's cyst.
He wasn't keen on the surgical intervention; thus, he decided to try pure expanded stem cell therapy in December 2018. He was then reviewed at the end of February 2019 and reported that he was delighted with the progress. He was pain-free, and his right knee had a full range of movement with no swelling or any tenderness. The report MRI in August 2019 showed some improvement and no further progression of his knee pathology.
He remains pain-free with normal knee movement—no need for any pain medicine and attending the gym regularly. No surgery will be required with an excellent long term prognosis given the therapy was delivered early, and he is a young person with good regenerative ability.
By Dr Hassan Mubark
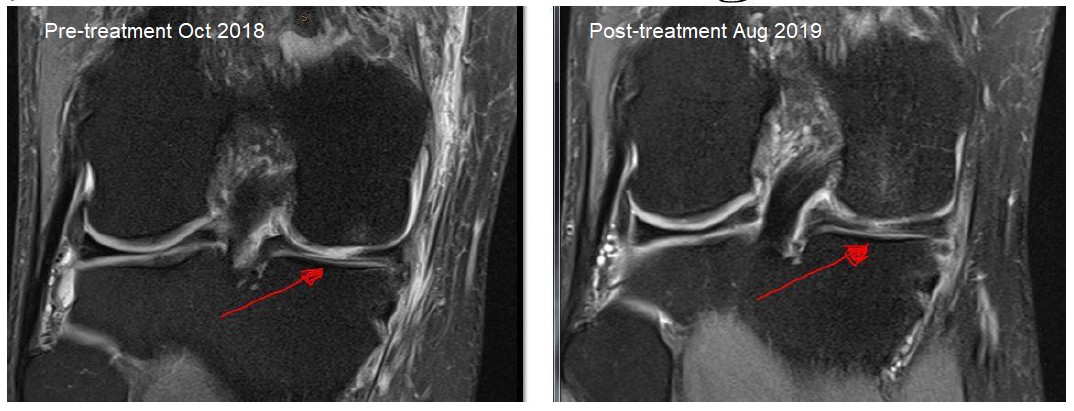
A 70-year-old woman with the regeneration of Full-Thickness Supraspinatus Rotator Cuff Tendon Tear after Treatment with Autologous Mesenchymal Stem Cells
Dr Mubark published this case study in a well known medical journal. Go here for the article.
Abstract
Rotator cuff tear (RCT) is primarily a disease of middle-aged and older patients. Observational data estimated linear increment in the frequency of RCT over time due to the degenerative process. However, a good proportion of tears in older patients are asymptomatic and do not require any intervention. Sport and non-sport Injuries can contribute to RCTs. Many RCTs can be treated non-surgically with anti-inflammatory medication, steroid injections, and physical therapy for symptomatic relief and to restore shoulder strength and function. Rotator cuff tendon tears have limited ability to heal independently, and most often, surgical repair is recommended in people failing non-operative therapy. The recovery time after surgery can be a lengthy process.
There are no conclusive data to support the routine use of biologic therapy like mesenchymal stem cells (MSCs) or platelet-rich plasma (PRP) in the treatment of symptomatic RCTs. Herein we report a full-thickness supraspinatus tear (SST) in an elderly patient’s shoulder following three injuries. The tear was confirmed by ultrasound scan (USS) and magnetic resonance imaging (MRI) with SST of 9 mm in length and 13 mm in width, unresponsive to anti-inflammatory medicines, rehabilitation, and steroid injections. The subject, however, did have a definitive clinical and radiological response to a single therapeutic injection using autologous adipose tissue-derived MSCs combined with PRP; the injections were performed by ultrasound guidance into the subacromial bursa, supraspinatus tendon and tendon insertion, respectively.
After five months, a USS showed some healing of the SST. Eight months post-MSC therapy, the subject had significant improvement in symptoms and dramatic improvement of the Disability of the Arm, Shoulder and Hand (DASH) score from a baseline of 88.3 before the therapy to 16.3 final visit. A Follow-up MRI scan revealed complete healing of the SST, indicating the possible successful MSC therapy outcome as an alternative non-surgical treatment.
The patient was cured without surgery.